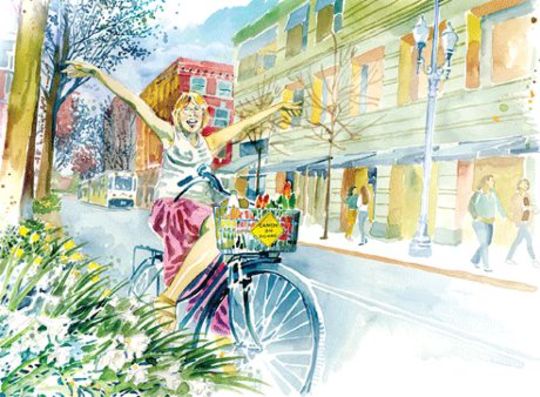
 Illustration by Julie Notarianni.
Illustration by Julie Notarianni.
"I pedal everywhere, slowly, on a bike that announces 'Cancer on Board.' I defy every attempt to limit me to my diagnosis as I dare the wold to ignore it."
Dying inevitably follows living. What makes for a good death in a just and sustainable world? I think about this a lot these days. Four years ago, at age fifty, I was diagnosed with late-stage ovarian cancer. Active and fit, it took a collapsed lung and two broken ribs before I realized I had a big problem, the ultimate challenge of life: facing my own death.
I defy every attempt to limit me to my diagnosis
as I dare the world to ignore.
In the first weeks after learning I was terminally ill, I wondered, “Will I face this in my heart or in my head? In my head, it is a storyline I can make interesting, wise, and abstract. In my heart, it is a constant tremor radiating from my stomach.”
As the first months of terror subsided, I began to adapt to my “new normal.” My medical team advised, “You must start living as if the next three months are your last. When you are still alive at the close, make a new three-month plan.” I resolved to hope and dream and build in smaller allocations of time.
I made huge shifts in my life, severing two critical anchor points. I moved to the city from the small town that had been my home for 25 years—my isolated existence in the woods seemed too daunting for the emotional swings of terminal cancer. I retired from the organization I had founded and that had been my life’s work for 18 years. I knew the long hours and stress of the job I loved would deplete the strength I needed for cancer treatment.
I qualified for Social Security disability income thanks to the government’s “compassion clause,” and this got me Medicare two and a half years later. I stepped into my new life determined to live as long as possible. I decided I would live to be 72 years old, 19 years longer than the statistics predicted and an age I found acceptable to die.
Living Fully Even While Facing A Death Sentence
It’s estimated that one in three people in the United States will receive a cancer diagnosis at some point in life. Some people die quickly. Others diagnosed as terminal continue to live fully even while facing a death sentence.
A friend who had watched her mother die of cancer remarked on my vivacity. In the 15 years since her mother’s death, there have been advancements that make the devastating side effects of treatment more tolerable. Still, it has taken me years after my diagnosis to re-embrace the commitments that populate a full life.
I chafe at being invisible as a person with cancer. I am a lifelong feminist and community organizer. I believe in breaking silence and sharing truth. I pass as “normal”—healthy, white, slender, and heterosexual (having a husband helps). I have lived a life of privilege. For now, I don’t look or feel like I’m dying. I am just terminally ill.
Recently I was reminded of the great Rachel Carson. She hid the pain of her end-stage cancer to keep her Silent Spring message of environmental degradation alive in Congress and mainstream conversation back in 1964.
In 2014, I can choose to be visible. I have a tattoo on my wrist declaring me a “Cancer Warrior.” I sport buttons saying “Cancer Sucks.” I pedal everywhere, slowly, on a bike that announces “Cancer on Board.” I defy every attempt to limit me to my diagnosis as I dare the world to ignore it.
We have little choice but to live in the moment;
something many talk about, but few manage.
But sometimes I feel I am as isolated in shouting about my diagnosis as Rachel Carson was in secrecy. I look so good that observers may well conclude that the sign on my bike, the button on my bags, even the tattoo on my wrist represent strength and survival.
Public or private, silent or loud, the outcomes are the same. Disease creates isolation and barriers from the world of the well. A friend with terminal cancer notes,
“We cause discomfort to some because we are living, living in acute awareness of our impending death, living in pain but living as fully as we can while we are dying. Should we lock ourselves away in a figurative darkened room so as not to chance disturbing the hale and hearty with thoughts of death?”
People say odd things when they attempt to comfort the terminally ill while avoiding their own fears. “We are all terminally ill. You just know it.” I more than “know it” as my weary veins dodge yet another dose of chemotherapy, toxic poison that will bring me to my knees with exhaustion, nausea, and brain fog while hopefully keeping me alive a while longer.
While the statistics gave me little hope, real people with cancer provide inspiration. They look normal and live well. They laugh, watch TV, and travel. They haven’t stopped living, even as medical appointments, surgeries, treatments, and side effects disrupt their days.
Finding Your Support Circle
I sought out other women living with a pink slip from life and discovered how hard it is for us to find each other. Medical privacy laws don’t help. Advocacy groups are often Web- or hospital-based, but not everyone flourishes in those settings. Eventually I created my own support circle of other women with terminal cancer.
The group is called “It’s a Dying Shame,” and the outreach flyer states, “Our goal is to explore the rich and peculiar territory of facing our own deaths. Together we can mine the humor, strangeness, and beauty of a life turned upside down. Join us for tea down the rabbit hole.” Our group meetings provide a cherished time to speak our truth without taking on the emotions of friends and family.
People often say to the terminally ill, “You are so stoic, so graceful. I could never handle this so well.” Perhaps not. The truth is you have no idea how well or badly we, the dying, handle it. Kim, diagnosed as terminal three years ago at age 34, says,
“Each day can vary greatly. Is it a doctor appointment day? Scan day? A day of total rest and relaxation? A day that the thought of me dying before age 40 leaves me immobilized, weeping in bed, and tightly grasping a heating pad? In a month’s time I go through all of these typical days. And then some.”
The Journey Toward Death
Social media also allows us to communicate with new ease about approaching death. Thousands follow Lisa Adams’ blog, where she describes every aspect of the medical and emotional realities of facing death as she copes with raising a young family. She doesn’t make it look easy or pretty.
Lisa and other dying bloggers offer a view of pain that is normally rarely witnessed and ask that people with terminal cancer be seen as more than “courageous.” Guardian columnist Emma Keller and her husband chided Adams for over-sharing. I think that those who condemn our process are distancing themselves from Lisa—and me—and from the reality of protracted death.
The current rules of polite conversation make the journey toward death more challenging. One woman said to me, “It is like we are standing in a different room.” We are avoided or jollied up. (“You look so good you can’t be terminally ill” is the most hated and common of compliments.) These approaches insulate people in our culture from sitting with death, sadly but comfortably.
When people with terminal diagnoses communicate about their experience, it may make their walking toward death more doable. I cannot think of subjects better suited for full honesty than birth and death.
Reframing Terminal Cancer as a Chronic Disease?
There is a trend to reframe some terminal cancers as a chronic disease, perhaps to avoid mention of death, to give hope, or because some terminal diseases are becoming more manageable over the years. One woman in her 40s rejected that label after six years in treatment:
“For most people, it makes sense to make plans beyond one month at a time, but even that short a time-frame can turn out to be optimistic for me. Unexpected side effects catch up with me; treatments that we thought were working cease to work months earlier than expected, and suddenly we are thrust again into making life-and-death decisions, lacking any real information about what may—or may not —buy me even a few more months of life. Making plans in this context becomes almost a joke. Something about this state that I live in seems really different to me from what I think of as chronic illness. It is more like a slow dying process, during which I get to LIVE.”
I have noticed many of us with terminal cancer are of good cheer and even invigorated by having no presumption of longevity. We have little choice but to live in the moment; something many talk about, but few can manage. When you live treatment to treatment and test result to test result, there is less room for distraction by petty stresses. We can’t expect to live another year, but if we do survive one year, or five, or ten, we consider ourselves very lucky. My mandate is to live with the shadow of death seated comfortably on one shoulder—I rarely forget, but I often dismiss, my new companion.
Dying Is Woven Into The Reality Of Living
I have made a certain peace with leaving this world, a peace experienced only after pondering what I might do, where I might be, what I might become after I die. I live in a culture that offers few views of what happens after death—it is either THE END (humus for the ages), or it is some mythic version of heaven and hell. Neither option works for me. I imagine my next world as Peter Pan did, “To die will be an awfully big adventure,” even if his image of death is more boisterous than mine.
Weeks after my diagnosis, before relocating to the city, I sat in the spring sunshine by a creek at our homestead while my sweetie did the chores I couldn’t do post-surgery. This was a favorite spot of mine. The chickens made comforting clucks in their enclosure to my right while the ducks quacked comically in the pasture to my left. The warmth of the sun reached every nook of my body. I was surrounded by so much that I loved—the tears I cried were happy ones. Couldn’t this be my heaven?
Today, I live in a lovely neighborhood, in a lovely house surrounded by pleasures that don’t take away the sorrow of departure. My life stays filled with joy and meaning as well as sadness and grief. I am livingly dying. Dying is woven into the reality of living. Neither is easy. But just as we live as a community, let’s face death as a community too.
This article was first published in YES! Magazine.
About the Author
 Marcy Westerling wrote this article for The End of Poverty, the Fall 2014 issue of YES! Magazine. Mary is a long-time community organizer with a passion for justice. She founded the Rural Organizing Project (ROP) in 1992. She is currently on her seventh approach to stabilize her cancer. She blogs at livinglydying.com.
Marcy Westerling wrote this article for The End of Poverty, the Fall 2014 issue of YES! Magazine. Mary is a long-time community organizer with a passion for justice. She founded the Rural Organizing Project (ROP) in 1992. She is currently on her seventh approach to stabilize her cancer. She blogs at livinglydying.com.
Recommended book:
Being Well (Even When You're Sick): Mindfulness Practices for People with Cancer and Other Serious Illnesses
by Elana Rosenbaum.
 The simple techniques Elana Rosenbaum presents here are the same ones she uses with the people in her practice of mindfulness-based psychotherapy and stress reduction—and that she uses herself as a cancer survivor. These are methods that offer proof positive that it is indeed possible not only to “have a life” while you’re seriously ill, but that the life can include satisfaction, ease, and happiness. This book includes a downloadable companion 60-minute audio program with seven simple mindfulness practices.
The simple techniques Elana Rosenbaum presents here are the same ones she uses with the people in her practice of mindfulness-based psychotherapy and stress reduction—and that she uses herself as a cancer survivor. These are methods that offer proof positive that it is indeed possible not only to “have a life” while you’re seriously ill, but that the life can include satisfaction, ease, and happiness. This book includes a downloadable companion 60-minute audio program with seven simple mindfulness practices.
Click here for more info and/or to order this book on Amazon.