A new analysis of the medical records of more than 5.5 million older adults admitted to nursing homes between 2011 and 2014 shows that those with delirium face an increased risk of death. They’re also more likely to be readmitted to the hospital.
“Upon admission to post-acute care, there are at least 4 percent of patients who have delirium,” says Cyrus Kosar, a graduate student at Brown University who led the research and presented the results at the Academy Health Annual Research Meeting in Boston. “We should make an effort to improve care for these specific patients since they are high risk.”
Delirium is sometimes misunderstood, even among health care providers. It’s not chronic, which is a key distinction from dementia.
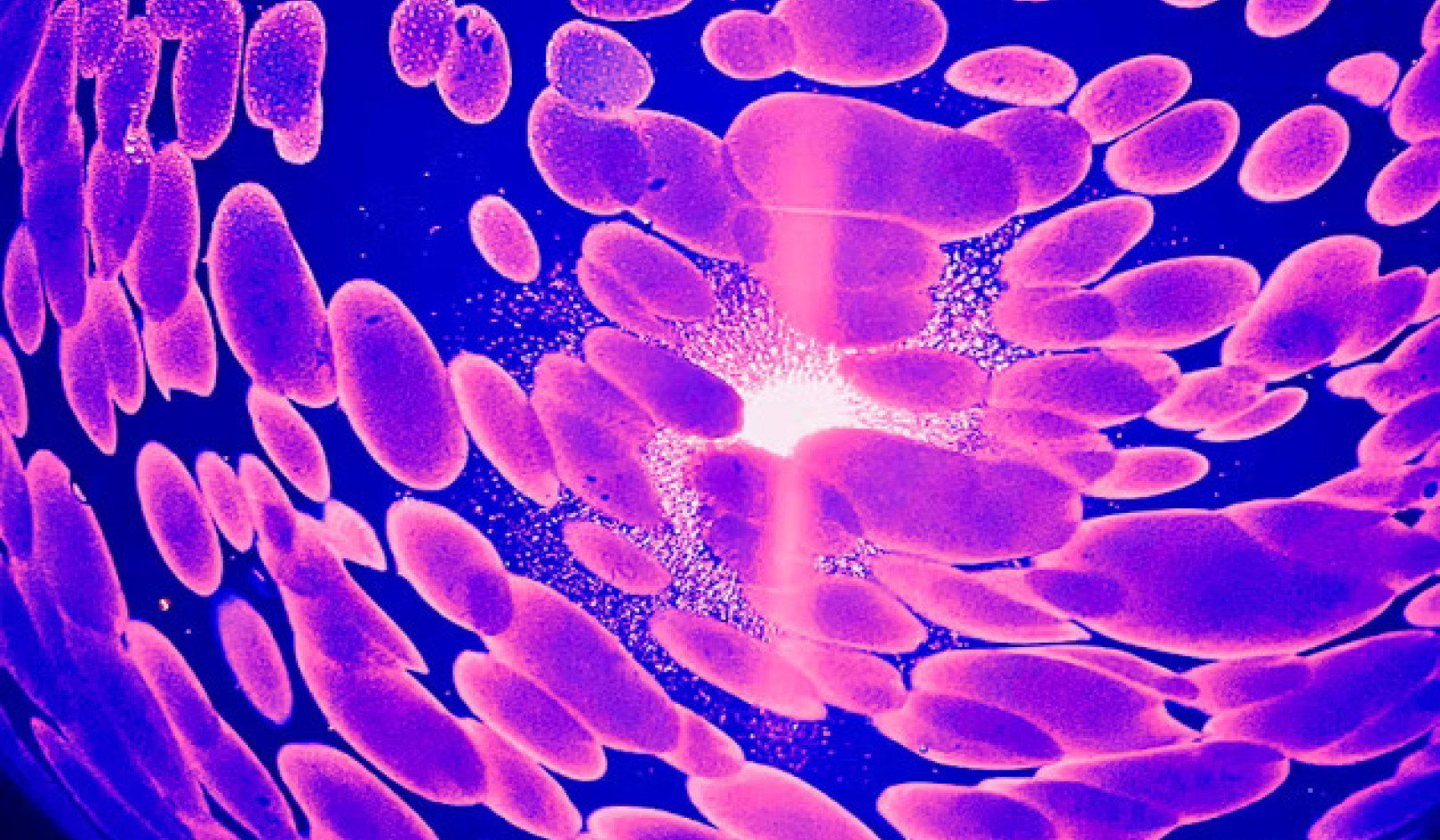
Delirium is sometimes misunderstood, even among health care providers. Often observed among hospitalized patients—particularly older ones—it’s an acute decline in cognitive functioning that may appear to come and go, sometimes within matters of hours. It’s not chronic, which is a key distinction from dementia, a long-term, progressive, terminal degeneration of brain function.
The condition may result from severe illnesses such as lingering infections, dehydration, sedation, or an improper blending or administration of medications.
“Delirium essentially is a good signal of a sicker patient or for a patient who is not getting the care that they need,” says Kosar, who worked with Vince Mor and Kali Thomas from the School of Public Health.
Other researchers have found that health outcomes among patients with delirium are worse while they are in the hospital than for people without delirium. In this case, Kosar and Thomas wanted to look into the impact of delirium on post-acute care outcomes.
“There is a good chance that the patients who are admitted to post-acute care with delirium came from acute care with delirium, so we might be capturing a group of patients with unresolved delirium,” Kosar says.
Researchers performed the analysis by looking at the national dataset of nursing home care, which recently began requiring structured assessments of delirium. To compile the records, nursing home personnel measured a variety of demographic and health characteristics in incoming patients, including delirium using the standard Confusion Assessment Method. In all, their sample included 5.58 million patients aged 65 or older admitted to nursing homes for post-acute care.
Of all the patients, more than 1.1 million had dementia, but even after a statistical accounting for that form of cognitive decline and other health problems (as well as age, gender and other factors) the patients with delirium faced greater health risks.
The mortality rate after 30 days was 16 percent among those with delirium compared to 6 percent (a statistically adjusted 2.3 times greater risk). The risk of readmission to the hospital within a month was also higher: 21 percent for seniors with delirium vs. 15 percent among those without (a 1.4 times risk).
Among those delirium patients who went home after the nursing home admission, their rate of functional recovery (a decrease in dependency for daily living activities as measured by a standard scale) was lower: 49 percent vs. 60 percent (a statistically adjusted 17 percent lower chance).
The researchers say the findings could help nursing home care providers be aware that a significant number of their patients likely arrive with delirium and that the stakes for those patients are especially high. Identifying and addressing it could save lives and spare patients (and their insurers) from unnecessary readmissions to the hospital.
Source: Brown University
Related Books
at InnerSelf Market and Amazon